In 2026, navigating the financial complexities of healthcare is more challenging than ever. With reimbursement models evolving, payer rules shifting, and staffing pressures mounting, managing the revenue cycle efficiently isn’t just a back-office function. It’s a strategic imperative. Healthcare providers need partners that not only understand the technical intricacies of billing but can also adapt in real time to regulatory changes and payer behavior.
That’s where specialized healthcare revenue cycle management (RCM) companies come in. These firms combine deep domain expertise with powerful technology to streamline the patient-to-payment journey, reduce denials, and accelerate cash flow. As health systems and medical practices look to maximize revenue while minimizing administrative burden, choosing the right RCM partner can make a major difference.
Below, we explore the top 10 healthcare RCM companies to watch in 2026, ranked by their innovation and the breadth of their feature offerings.
Top 10 healthcare RCM companies for 2026
1. Aptarro
3. Optum
4. R1 RCM
5. GeBBS
6. Epic Systems
8. Athenahealth
10. Conifer Health
What Is Healthcare RCM?
Healthcare Revenue Cycle Management (RCM) is the end-to-end financial process that healthcare providers use to manage and optimize the flow of revenue associated with patient services. It begins at the moment a patient schedules an appointment (or even before, during pre-registration) and continues all the way to final payment, whether that comes from the insurer, the patient, or both. This process is a critical bridge between clinical care and financial operations, ensuring that services rendered are accurately captured, billed, and collected.
RCM is inherently complex because it spans both administrative and clinical domains. On the administrative side, it includes patient registration, insurance eligibility verification, and financial counseling. On the clinical side, it involves translating documentation into billing codes, ensuring compliance, and capturing all billable services. In addition, RCM covers claims submission, denial management, payment reconciliation, and ongoing accounts receivable (AR) follow-up.
Because of the many steps involved, even small inefficiencies can compound and create revenue leakage. That’s why strong RCM is not just about billing correctly; it's about creating a streamlined, predictable financial operation that supports both patient care and the provider’s financial health.
Here’s a simplified look at the typical phases of RCM and their core activities:
| Phase | Key Activities |
| Pre-service | Patient scheduling, registration, insurance verification, and authorization |
| Service/Clinical | Charge capture, medical coding, and documentation of services |
| Post-service | Claims submission, payment posting, denial management, and patient collections |
By breaking RCM down into these phases, providers can see where revenue may be at risk. For example, a denial spike may point to problems in post-service, while billing delays could start in pre-service. Effective RCM ensures that each phase flows into the next with minimal friction, reducing errors and maximizing reimbursements.
What Is a Healthcare RCM Company?
While healthcare RCM describes the process, a healthcare RCM company is an external partner that helps execute, optimize, or manage that process. These companies offer specialized expertise, technology, or both, allowing healthcare organizations to outsource or enhance parts of their revenue cycle rather than handling everything in-house.
RCM companies vary widely in their business models and service offerings, depending on the needs of their clients. Some are pure-software providers, delivering cloud-based or on-premises platforms that automate billing, coding, denial workflows, and analytics. Others are fully managed services: staffed teams that take over billing, AR follow-up, denial appeals, and more. Still others adopt a hybrid model, combining smart automation with human expertise.
To illustrate how these models differ, consider the following breakdown:
| Type of RCM Company | What They Provide |
| RCM software provider | Platforms to automate billing, coding, claim scrubbing, denial prevention, and analytics. |
| Managed services/Outsourcing | Dedicated teams handling registration, billing, collections, denials, and appeals. |
| Hybrid model | A combination of both: software and expert staff who use it to manage complex RCM tasks. |
Choosing the right type of RCM company depends heavily on a provider’s internal capacity, financial goals, and risk tolerance. For example, a smaller clinic with limited staffing might benefit from a fully managed service, while a large hospital system may prefer a software-first partner that augments its internal teams.
By partnering with an RCM company, providers gain access to specialized skills, scalable infrastructure, and advanced technology — all without bearing the full burden of building and maintaining those resources themselves. This can lead to more predictable cash flow, fewer write-offs, and a more efficient revenue cycle.
Top 10 Healthcare RCM Companies for 2026
1. Aptarro
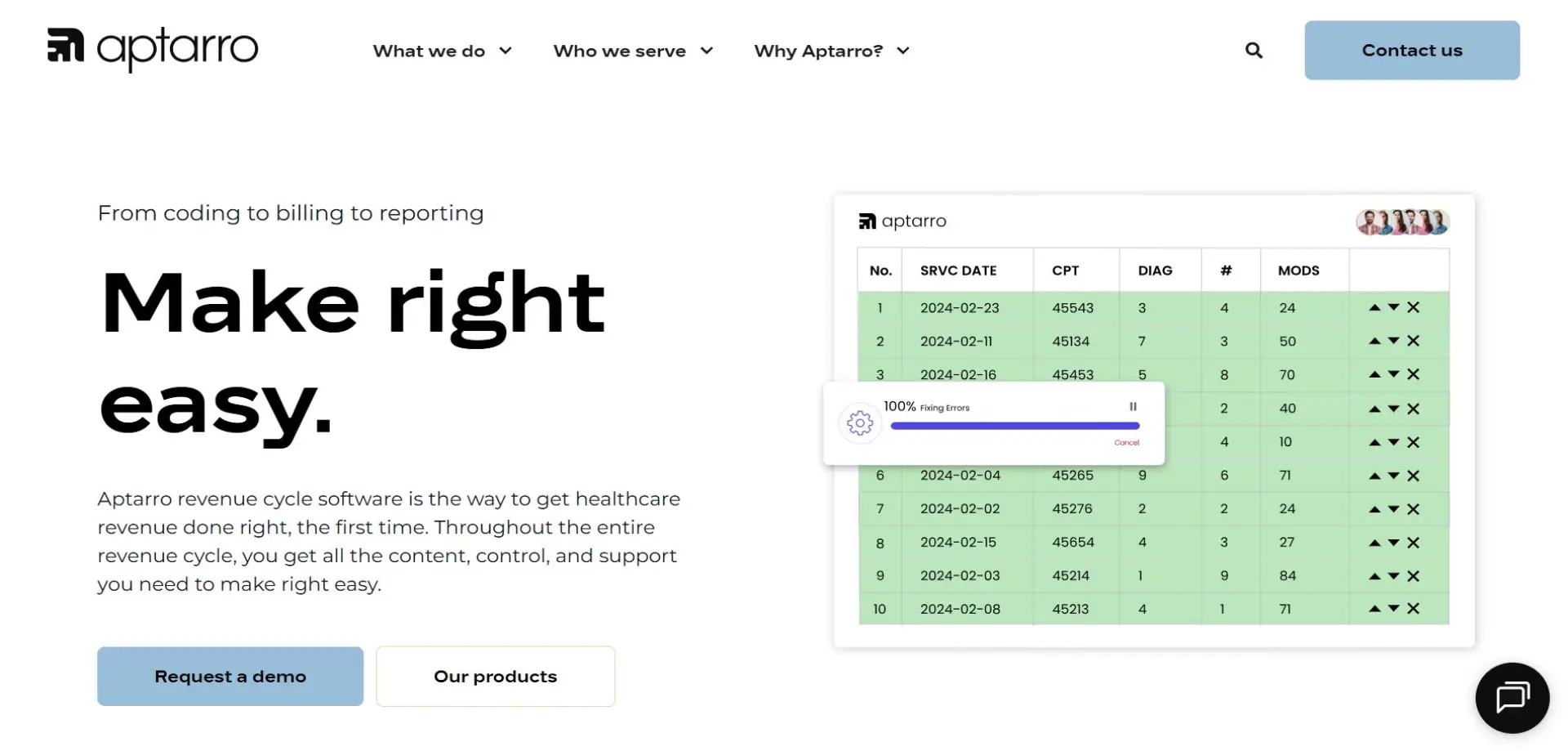
Aptarro stands out as a leading healthcare RCM company, known for its innovative RevCycle Engine. The platform serves as a central hub for managing revenue cycle processes, helping providers improve accuracy and efficiency across their financial operations. Aptarro’s software is designed to integrate smoothly with existing electronic health records (EHRs) and practice management systems, offering a cohesive solution that supports healthcare organizations of all sizes.
Beyond its core platform, Aptarro emphasizes a philosophy of making revenue cycle management as simple and effective as possible. By combining intelligent automation with deep industry expertise, the company helps organizations streamline administrative workflows, reduce manual effort, and maintain strong financial performance. This allows staff to focus on patient care.
Aptarro’s solutions are flexible and scalable, serving large hospital systems, specialty practices, and everything in between. Its platform provides a reliable foundation for optimizing revenue cycle operations without overcomplicating the process. If you’re ready to explore how Aptarro can enhance your organization’s revenue cycle, book a demo today to see the platform in action.
2. NextGen Healthcare
NextGen provides both EHR and RCM solutions focused on small to mid-sized practices. Its revenue cycle services include billing, claims management, and analytics, helping practices optimize collections while minimizing administrative burden.
3. Optum
Optum provides end-to-end RCM services, including pre-registration, coding, billing, payer contract optimization, and analytics. Its scale and integration with the broader UnitedHealth Group ecosystem make it a strong choice for health systems seeking comprehensive and connected revenue cycle solutions.
4. R1 RCM

R1 RCM is a leading provider of outsourced revenue cycle services, handling tasks such as patient registration, billing, coding, denial management, and underpayment recovery. The company supports large health systems and is recognized for its operational scale and reliability.
5. GeBBS

GeBBS Healthcare Solutions delivers outsourced RCM services for hospitals, health systems, and physician groups. The company supports core functions like coding, billing, and AR management, offering scalable operational support that helps providers stay efficient and maintain financial stability.
6. Epic Systems
Epic is primarily known for its EHR, but it also provides robust embedded RCM tools. These tools offer tight integration with clinical workflows, seamless data flow, and consistent operations, making Epic a popular choice for large hospital systems.
7. Oracle Health
Oracle Health provides integrated clinical and financial systems, including RCM modules tailored to large hospitals. Their platform enables health systems to manage both clinical and financial operations within a single ecosystem.
8. Athenahealth
Athenahealth’s athenaOne platform combines EHR, practice management, billing, and RCM, making it particularly suited for ambulatory practices and physician groups. Its cloud-based model allows for scalability and continuous updates.
9. Greenway Health

Greenway Health offers integrated EHR, practice management, and RCM solutions. Its RCM services are designed to support ambulatory practices with specialized financial care teams and tools that improve coding accuracy and cash flow.
10. Conifer Health
Conifer Health is a long-standing RCM outsourcing provider that helps hospitals and health systems with patient access, denial management, and revenue optimization. Their managed service model is particularly valuable for organizations seeking full-scale support and operational efficiency.
Benefits of Partnering with a Healthcare RCM Company
Partnering with a specialized RCM company brings several advantages. When done right, it’s not just about collecting what you’re owed but about transforming your financial operations into a strategic asset.
Improved financial performance and predictability
By outsourcing or leveraging advanced RCM technologies, providers can significantly reduce denials, accelerate payments, and optimize their reimbursement pipeline. This leads to more consistent cash flow and fewer surprises in the financial statements.
Reduced administrative workload
RCM companies take over complex and labor-intensive tasks (from claims follow-up to appeals), allowing provider organizations to redeploy internal staff toward higher-value work such as patient care.
Enhanced data insights and decision-making
Leading RCM providers offer dashboards, analytics, and rule-based intelligence that illuminate trends in payer behavior, denial patterns, and revenue leakage. These insights enable proactive interventions and continuous process improvement.
Scale and flexibility
Whether you are a solo clinic or a multi-hospital system, RCM companies can scale their support to meet your needs. Their modular and hybrid models make it possible to pick and choose where you need help most: be it front‑end automation, back‑office services, or both.
Key Features of a Healthcare RCM Company
Here are some of the critical capabilities that top-tier RCM companies bring to the table. These features drive value and differentiate the best partners in the market.
Real‑time eligibility and benefits verification
A modern RCM provider often includes real-time insurance checks at patient intake, ensuring that coverage, copays, and prior authorization requirements are validated upfront. This works to reduce denials and surprise patient balances.
Automated charge review and correction
Using rules-based technology (often with AI or machine learning), RCM platforms can review clinical encounters or flags for potential coding or charge issues before claims are generated. This improves claim accuracy and reduces costly rework downstream.
Denial management and appeals workflow
High-performing RCM providers don’t just alert you to denied claims. They categorize them, automate appeals, and provide visibility into root causes. This helps to prevent repeat denials over time.
Payment posting and reconciliation
Once a claim is paid, RCM systems help reconcile payer remittances or patient payments, apply them to the correct accounts, and flag any discrepancies. The result is reduced errors and less need for manual effort.
Financial analytics and reporting
Top RCM companies provide real-time KPIs (denial rate, days in AR, net collection rate) and predictive reporting. These metrics empower providers to make data-driven decisions and forecast financial health more accurately.
Patient financial engagement
Some RCM firms also support patient-facing tools (such as portals, statements, and payment plans), helping to engage patients in their financial responsibilities and improving collections.
What to Consider When Choosing a Healthcare RCM Company
Selecting the right RCM partner is a strategic decision. Here are the key factors to evaluate:
Strategic alignment and service model
First, decide whether you need a technology-only partner (just the software), a fully managed-services partner (they handle everything), or a hybrid. What fits best depends on your internal capabilities, risk appetite, and long-term goals.
Integration and interoperability
Ensure that the RCM solution integrates smoothly with your current infrastructure: EHR, practice management, and clearinghouse systems. Strong integration reduces friction, improves data accuracy, and accelerates adoption.
Scalability and flexibility
Choose a partner that can grow with you. Whether you expand to new specialties, geographic locations, or service lines, the RCM partner should offer a modular and scalable model.
Compliance and security
RCM involves sensitive patient and financial data. Confirm that your partner is compliant with regulatory standards (e.g., HIPAA in the U.S.) and has robust security controls, data governance, and audit capabilities.
Pricing model and transparency
Get clarity on how the provider charges: Is it volume-based, a percentage of collections, or a flat rate? Understand how costs change as your claim volume or payer mix evolves.
Vendor support and partnership
Evaluate the onboarding process, training, account management, and ongoing optimization support. Strong RCM partners act as long-term collaborators, not just vendors.
Optimizing Your Revenue Cycle for Better Results
In a healthcare environment where payer rules are more complex, patient out-of-pocket costs are rising, and the administrative burden is growing, optimizing the revenue cycle is no longer a back-office luxury. It’s a strategic imperative. The right RCM partner can transform your revenue operations from a cost center into a competitive advantage.
When you work with a trusted provider like Aptarro, you gain access to sophisticated automation via RevCycle Engine, expert rules-based review, and a deep bench of domain knowledge.
If you’re ready to take control of your revenue cycle and drive measurable financial outcomes, book a demo with Aptarro today. Let our experts show you how to make "right" easy.
Author
