In today’s fast-paced healthcare environment, providers are under increasing pressure to manage claims efficiently while maintaining compliance and accuracy. Manual claims processing is often time-consuming, prone to errors, and can lead to delayed reimbursements, denials, and revenue loss. Automated claims processing solutions have emerged as a key strategy for healthcare organizations looking to streamline workflows, reduce administrative burden, and accelerate revenue cycles.
Automated claims processing integrates technology, digital workflows, and sometimes AI-driven tools to handle the full lifecycle of a claim. This can include everything from verifying patient eligibility to submitting claims, monitoring approvals, and posting payments.
As adoption grows, healthcare organizations are evaluating software solutions that can scale with their operations, integrate with existing systems, and provide reliable reporting and analytics. Below, we present the top 10 automated claims processing software platforms for 2026, followed by insights into their benefits, key features, and what to consider when selecting the right solution for your organization.
Top 10 automated claims processing software for 2026
1. Aptarro
2. Waystar
3. Availity
4. Optum
5. TriZetto Provider Solutions
7. FinThrive
8. R1 RCM
10. SSI Group
What Is Automated Claims Processing?
Automated claims processing is the practice of using technology to handle insurance claims with minimal human intervention. It focuses on improving the speed, accuracy, and efficiency of submitting, tracking, and reconciling claims while reducing errors and administrative overhead. Unlike traditional manual processes, which involve paper forms and repetitive data entry, automated claims processing leverages digital workflows, rule-based systems, and sometimes AI to ensure claims are clean and compliant before submission.
This approach benefits healthcare providers by shortening reimbursement cycles, lowering the risk of claim denials, and freeing staff from repetitive tasks. By automating repetitive and error-prone steps, organizations can focus on patient care and operational efficiency while improving financial performance.
The following table outlines the main stages of automated claims processing:
| Stage | What it Involves |
| Eligibility verification | Confirming a patient’s insurance coverage before services are rendered. |
| Coding and claim preparation | Assigning accurate codes and preparing claims based on documentation. |
| Claim submission and transmission | Sending claims electronically to payers or clearinghouses. |
| Adjudication and payer response | Receiving approvals or denials and interpreting payer feedback. |
| Payment posting and reconciliation | Recording payments, remittances, and adjustments. |
By automating these stages, healthcare organizations reduce errors, improve first-pass claim acceptance, and create a more predictable revenue cycle. In the process, it lays the groundwork for smoother interactions between providers, payers, and patients.
What Is Automated Claims Processing Software?
Automated claims processing software is the tool or platform that enables the digital and automated workflows described above. While “automated claims processing” refers to the overall approach or strategy, the software is the practical means through which healthcare organizations implement this approach. It replaces manual claim handling with digital solutions that streamline, monitor, and optimize the entire claims lifecycle.
This software centralizes key processes, such as eligibility verification, claim submission, denial tracking, and reporting, into a single system. Beyond automation, it provides visibility into claim statuses, performance metrics, and potential bottlenecks, helping administrators make informed decisions to enhance financial outcomes.
Below is a table showing how automated claims processing software differs from traditional manual workflows:
| Traditional manual process | Automated software approach |
| Paper-based claim forms and manual data entry | Electronic submission with standardized digital forms |
| Manual insurance eligibility checks | Real-time eligibility verification through payer databases |
| Manual coding and claim review | Automated claim preparation and code verification |
| Manual follow-up on denials | Integrated tracking and workflow for resubmissions |
| Spreadsheet-based payment reconciliation | Dashboards and automated reporting for payment posting and accounts receivable (AR) management |
Automated claims processing software provides the infrastructure to implement automated claims processing effectively. It reduces errors, increases efficiency, and ensures compliance with payer and regulatory requirements.
Top 10 Automated Claims Processing Software for 2026
1. Aptarro
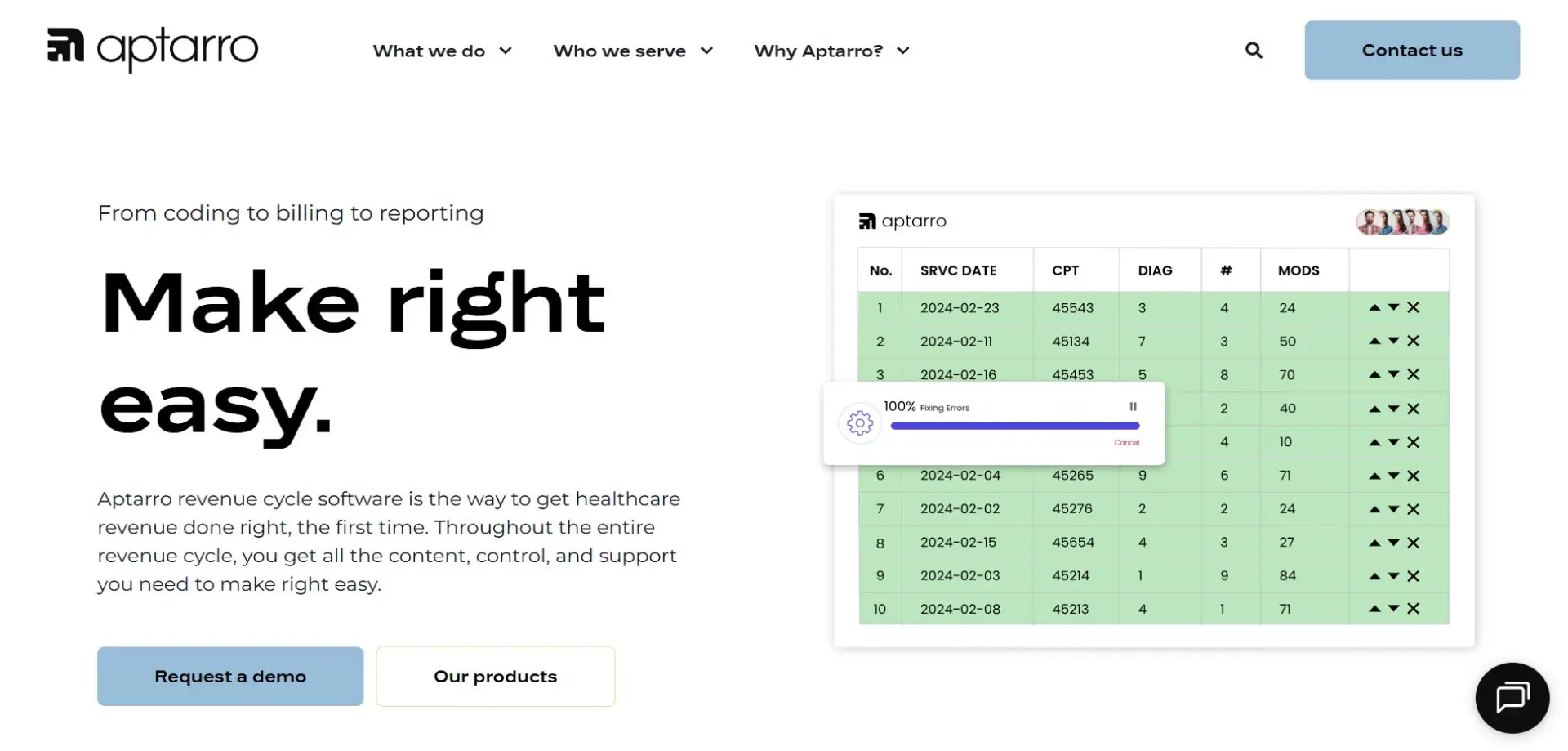
Aptarro stands out as a comprehensive revenue cycle management platform, offering robust support for automated claims processing through its RevCycle Engine. The platform is designed to optimize the end-to-end claims workflow and improve operational efficiency for healthcare providers. Its technology enables a streamlined approach to claim submission, monitoring, and reconciliation, helping organizations reduce administrative burden and improve revenue predictability.
The RevCycle Engine is known for its reliability and scalability, accommodating both small clinics and large hospital systems. Providers using Aptarro often report enhanced accuracy in their claim workflows and improved organizational oversight of the entire revenue cycle. Its comprehensive design helps healthcare organizations maintain compliance and adapt to changing payer requirements.
By integrating automated processes with user-friendly tools, Aptarro delivers a balance of technology and usability. The platform empowers staff to focus on high-value tasks, reduces human error, and supports faster reimbursement cycles. Discover how Aptarro’s RevCycle Engine can transform your claims processing and schedule a demo today.
2. Waystar
Waystar is recognized for its powerful automation and analytics capabilities in claims management. It simplifies claim submissions, improves visibility into claim statuses, and reduces the risk of denials. Healthcare organizations using Waystar benefit from streamlined processes and increased operational efficiency.
3. Availity
Availity is a leading platform for automated claims processing and clearinghouse management. It helps healthcare organizations streamline claim submissions, reduce errors, and improve workflow efficiency. Providers value Availity for its reliability, broad payer connectivity, and ability to support a variety of practice sizes.
4. Optum
Optum is widely adopted by healthcare providers for its robust claims processing and workflow management. The platform helps streamline claim submissions and ensures consistency across large health systems. Its robust approach supports efficient revenue cycle operations.
5. TriZetto Provider Solutions
TriZetto Provider Solutions is distinguished by its clearinghouse capabilities and claim management efficiency. The software helps organizations process claims accurately and quickly, providing clear visibility into the status of submissions. TriZetto is a trusted solution for organizations that want to prioritize both speed and accuracy.
6. Experian Health
Experian Health offers dependable claims management and payer connectivity. It helps providers maintain smooth workflows and reduces administrative overhead. Its platform is noted for its user-friendly interface.
7. FinThrive
FinThrive supports automated claim submissions and clearinghouse interactions. Providers appreciate its efficiency and integration with existing revenue cycle systems. The software helps organizations manage claims with greater consistency and speed.
8. R1 RCM

R1 RCM delivers a hybrid approach combining automation and managed services. The platform helps healthcare organizations streamline patient intake, claim submission, and denial resolution. R1 RCM supports improved operational efficiency and faster reimbursements.
9. eClinicalWorks
eClinicalWorks integrates claims management with EHR and practice management systems. The platform supports small to mid-sized practices by automating routine claim workflows and improving visibility across revenue cycle operations. It is valued for its unified approach.
10. SSI Group
The SSI Group remains a practical and reliable solution for electronic claim submissions. The software helps organizations maintain accurate workflows and manage payer connectivity effectively. SSI is particularly recognized for stability and ease of use in claims processing.
Benefits of Automated Claims Processing Software
Automated claims processing software brings significant advantages to healthcare organizations by enhancing efficiency, accuracy, and overall financial performance.
Improved claim accuracy and reduced denials
By minimizing manual entry and standardizing workflows, automated software reduces the errors that can lead to claim denials. This leads to higher first-pass acceptance rates and fewer resubmissions.
Faster reimbursement cycles
Automation shortens the time between service delivery and payment posting, supporting healthier cash flow and reducing days in accounts receivable.
Lower administrative burden and operational costs
By handling repetitive tasks, automated software allows staff to focus on higher-value activities, improving efficiency and reducing labor costs.
Better scalability and handling volume surges
Automated solutions adapt to fluctuating claim volumes without requiring proportional increases in staffing, supporting organizational growth.
Enhanced analytics and reporting
Dashboards and reporting tools provide real-time insights into claim statuses, denial trends, and revenue cycle performance, helping organizations make informed decisions.
Key Features of Automated Claims Processing Software
Understanding key features can help your organization choose the right solution for its needs.
-
Eligibility verification automation: Ensures patient coverage is confirmed in real-time, reducing rejected claims due to inactive insurance.
-
Claim scrubbing and coding support: Identifies potential errors before submission, improving the chances of first-pass claim acceptance.
-
Denial management and automated resubmission: Flags denied claims and streamlines resubmission workflows, reducing revenue loss.
-
Integration with other systems: supports seamless interaction with electronic health record (EHR) and payer networks, creating unified workflows and minimizing manual handoffs.
-
Real-time reporting and analytics: Provides visibility into claims performance, supporting data-driven decision-making and operational optimization.
What to Consider When Purchasing Automated Claims Processing Software
Selecting the right solution requires careful evaluation of technical and operational factors to ensure that it integrates well with your healthcare practice. Here are some of the main things to consider:
Integration and interoperability: Ensure the software connects smoothly with existing systems to avoid workflow disruptions or data silos.
Compliance, security, and payer coverage: Confirm the platform adheres to regulatory standards and connects reliably with all relevant payers.
Scalability and volume capacity: The solution should handle your current and projected claim volumes without performance issues.
Vendor support and updates: Access to strong customer support and regular updates is essential for maintaining compliance and optimizing workflows.
Cost structure and ROI: Evaluate licensing, implementation, and operational costs against potential efficiency gains and financial benefits.
Optimizing Your Revenue Cycle with Automated Claims Processing
Automated claims processing software is transforming how healthcare organizations manage revenue cycles. Platforms like Aptarro’s RevCycle Engine, Waystar, and Iodine Software provide efficiency, accuracy, and visibility, helping practices and hospitals reduce administrative burden and accelerate reimbursements.
Investing in automated claims processing tools enables organizations to focus on patient care while maintaining financial stability. To see firsthand how Aptarro’s RevCycle Engine can improve your claims workflows, book a demo today and explore the full potential of automation for your revenue cycle management.
Author
