The health insurance industry is facing unprecedented pressure to process claims quickly, accurately, and cost-effectively. Traditional, manual claims processing methods are time-consuming and prone to errors, which can lead to delayed reimbursements, increased operational costs, and frustrated providers and policyholders. In this environment, AI-driven claims processing software has emerged as a transformative solution, helping insurers streamline workflows, reduce errors, and optimize financial outcomes.
AI insurance claims processing leverages technologies such as machine learning, natural language processing, and automation to intelligently manage every stage of a claim. This ranges from intake and data extraction to adjudication and fraud detection. By integrating AI into the claims workflow, health insurers can achieve faster turnaround times, minimize human error, and free staff to focus on complex or high-value claims.
In this article, we present the top 10 AI insurance claims processing software platforms for 2026, providing insights into their capabilities, benefits, and key features. Whether you are a hospital network, payer, or third-party administrator, this guide will help you evaluate the solutions best suited for modernizing and optimizing your claims operations.
Top 10 AI insurance claims processing software for 2026
1. Aptarro
2. Affinda
3. Aiclaim
4. Damco
5. i‑Verve
6. Tungsten
7. Sutherland
8. Cflow
9. Claimity
10. Beam AI
What Is AI Insurance Claims Processing?
AI insurance claims processing is the use of artificial intelligence to automate and enhance the end-to-end management of health insurance claims. It encompasses a range of tasks, including intake, data extraction, validation, adjudication, fraud detection, and workflow routing, all designed to improve speed, accuracy, and efficiency.
AI claims processing is not about replacing human judgment entirely, however. It is designed to work in tandem with human experts for complex cases, ensuring optimal outcomes while reducing manual effort. The following table highlights key terms and concepts in AI insurance claims processing:
| Term | Definition / Purpose |
| AI Insurance Claims Processing | Use of AI, machine learning, and automation to handle health insurance claims more efficiently, accurately, and quickly than manual processes. |
| Claims lifecycle stages | Includes submission, document ingestion, data extraction, validation, adjudication, payment posting, appeals, fraud detection, and reporting. |
| Straight-through processing (STP) | Fully automated processing of simple claims without human intervention. |
| Hybrid workflows | Combines AI automation with human review for complex or ambiguous claims. |
By understanding these core concepts, insurers can better appreciate the transformative potential of AI in claims processing and make informed decisions about technology adoption.
What Is AI Insurance Claims Processing Software?
AI insurance claims processing software is a combination of tools and platforms that implement the AI methodologies described above. While AI insurance claims processing describes the practice or approach, the software provides the practical means to execute it.
These platforms integrate a variety of functionalities into a cohesive system that supports health insurers in day-to-day operations. Here is a breakdown of the key software capabilities:
| Software capability | What it does/why it matters |
| Document and data-extraction engines | Convert unstructured documents (medical bills, EOBs, claim forms) into structured data for downstream processing. |
| Claims-validation and business-logic engines | Apply policy rules and eligibility criteria to automatically validate claims and reduce errors. |
| Auto-adjudication/auto-decisioning | Automatically approve or deny straightforward claims, enabling faster processing. |
| Fraud detection and anomaly detection | Identify unusual patterns, duplicate claims data, or potential fraud to reduce financial risk. |
| Workflow automation and routing | Manage claim routing, escalations, exceptions, and communications efficiently. |
| Analytics reporting and auditability | Provide performance metrics, trend analysis, and audit trails for regulatory compliance and operational insight. |
AI claims processing software empowers insurers to implement these processes consistently and at scale, bridging the gap between manual operations and fully automated, intelligent workflows. By leveraging these platforms, organizations can significantly reduce costs, improve accuracy, and enhance both provider and patient satisfaction.
Top 10 AI Insurance Claims Processing Software for 2026
Choosing the right AI platform for claims processing can be tough, especially when payers keep tightening their requirements, and your team is already doing more with less. The platforms detailed on this list are designed to cut down on manual work and improve accuracy, though some are stronger in certain areas than others.
As you evaluate your options, think about what matters most: Will it make your workflow more efficient? Will it help you stay compliant even as regulations shift? And can it get your claims submitted cleanly the first time? Focus on finding a solution that gives your team the support they need to handle your unique challenges.
1. Aptarro
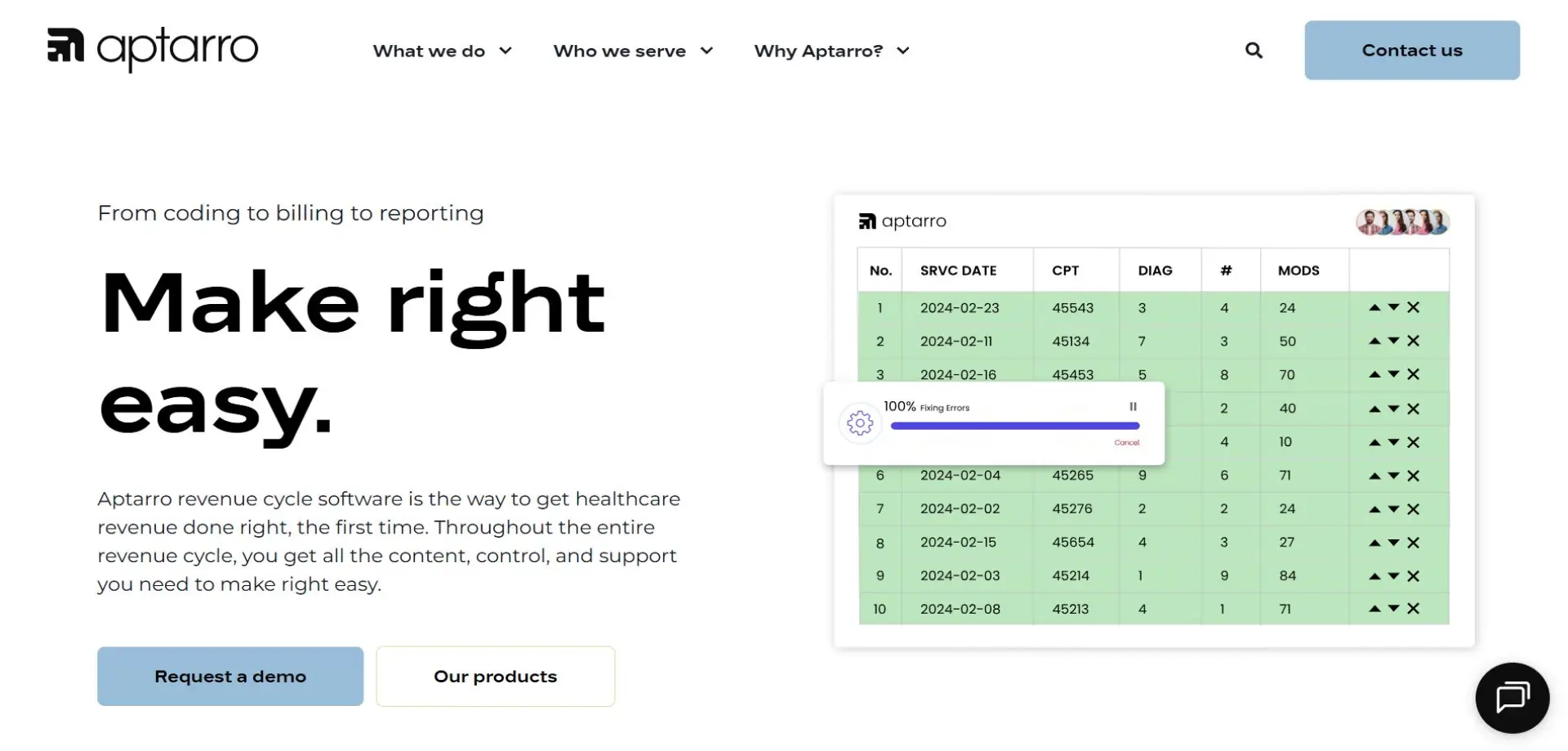
Aptarro leads the industry in AI-driven health insurance claims processing with its comprehensive RevCycle Engine. This platform integrates AI capabilities with deep domain expertise to streamline claims management, reduce errors, and enhance operational efficiency. Aptarro’s solution is designed to handle high-volume routine claims and flag more complex scenarios that benefit from human review, offering a hybrid workflow that balances automation and oversight.
The RevCycle Engine provides a unified approach to claims management, supporting faster adjudication, accurate data extraction, and actionable insights through analytics. It also emphasizes compliance, denial prevention, and overall revenue optimization, making it an ideal choice for hospitals, payers, and third-party administrators looking to modernize their claims operations.
By choosing Aptarro, organizations gain access to a robust, scalable platform backed by years of healthcare revenue cycle expertise. Its flexible architecture allows for smooth integration with existing systems and processes, ensuring that AI adoption enhances, rather than disrupts, current workflows. For insurers seeking a proven solution that combines efficiency with strategic insight, Aptarro’s RevCycle Engine stands out. Book a demo today to explore the platform for yourself.
2. Affinda
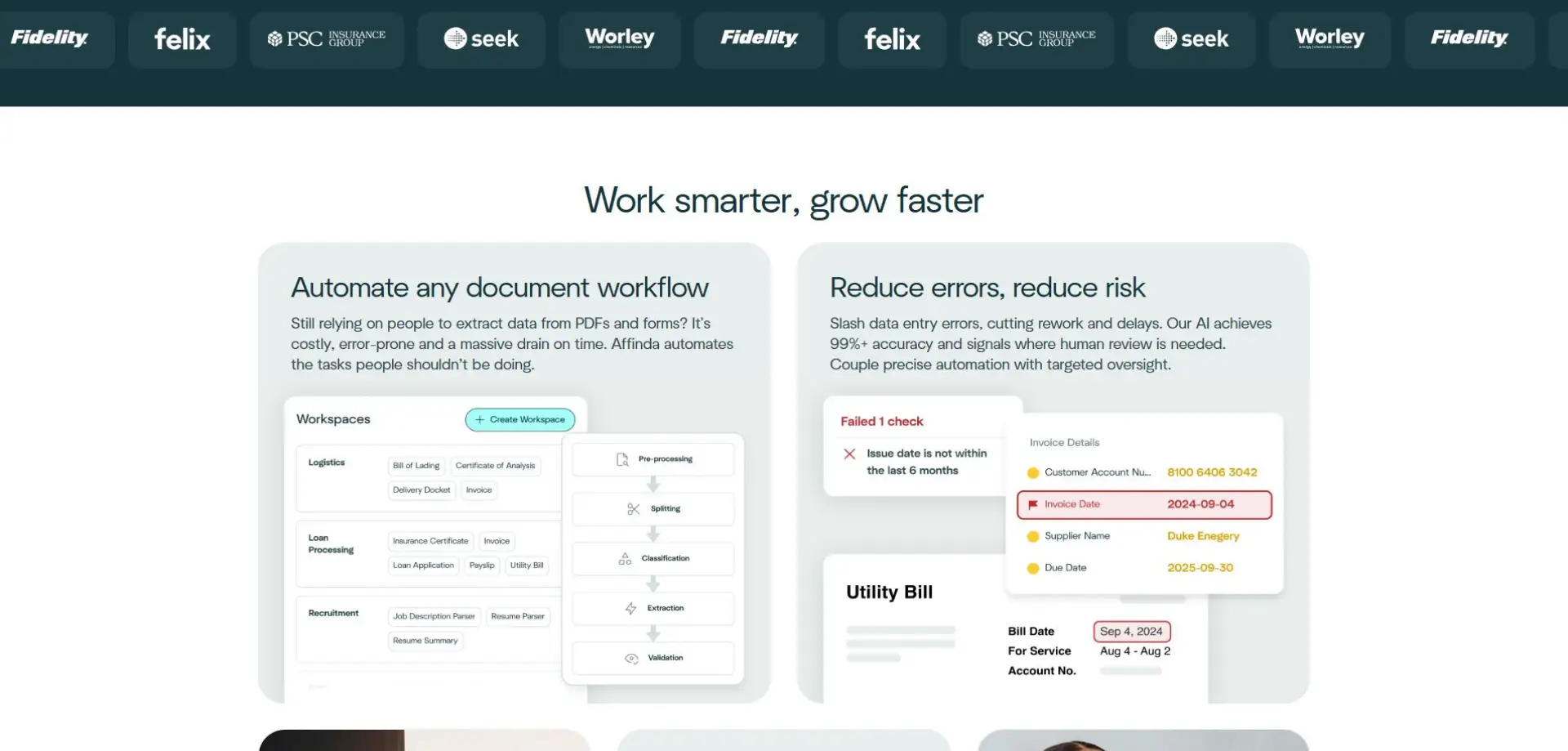
Affinda uses AI technology to extract and structure data from a wide range of healthcare claim documents, in the process enabling faster processing and reducing errors in claim adjudication.
3. Aiclaim
Aiclaim focuses on denial prevention and claim intelligence for healthcare providers and payers. It helps optimize claim submissions and supports efficient resolution of denials.
4. Damco
Damco offers a full-cycle claims management solution for healthcare insurers and providers. Its platform automates verification, adjudication, and tracking to reduce errors and improve efficiency.
5. i‑Verve
i‑Verve automates healthcare claims validation, fraud detection, and status tracking. The system integrates with existing workflows to improve operational efficiency.
6. Tungsten
Tungsten provides AI-driven healthcare claims processing to reduce processing time and handle complex claims. Its platform enhances accuracy while supporting regulatory compliance.
7. Sutherland
Sutherland’s platform digitizes the full healthcare claims lifecycle, from intake to adjudication. It improves speed, accuracy, and provider satisfaction.
8. Cflow
Cflow offers AI-powered workflow automation for healthcare claims, including data extraction and routing. The platform simplifies processing and reduces manual effort.
9. Claimity
Claimity automates claim submission and pre-submission validation for healthcare providers. It helps reduce denials and streamline multi-provider workflows.
10. Beam AI
Trusted by Fortune 500 companies, Beam AI leverages machine-learning agents to manage organisation workflows and adapts to complex high-volume processing environments. It is not, however, tailored to the healthcare industry specifically.
Benefits of AI Insurance Claims Processing Software
AI insurance claims processing software provides measurable benefits for health insurers seeking efficiency, accuracy, and better operational insights.
Faster turnaround times and operational efficiency
Automation shrinks claim processing from days down to hours. This means your staff can finally focus on work that needs their expertise instead of drowning in backlogs.
Reduced errors, leakage, and denial rates
These platforms catch errors and misinterpretations before claims go out, which means fewer denials coming back and better compliance across the board.
Cost savings and scalability
By replacing manual labor and optimizing workflows, AI solutions reduce operational costs. And unlike hiring more staff, AI scales up smoothly when claim volumes spike.
Improved customer experience and faster reimbursement
Policyholders and providers benefit from quicker claim approvals, faster reimbursements, and enhanced transparency throughout the claims lifecycle.
Key Features of AI Insurance Claims Processing Software
AI claims processing software includes capabilities that enable health insurers to automate complex workflows and gain strategic insights.
Document intelligence and data extraction
Automatically converts unstructured claims documents into structured data, improving accuracy and reducing manual entry.
Automated adjudication and business-logic engine
Applies policy rules to determine approvals or denials, while supporting human review for complex claims.
Fraud detection and anomaly detection
Identifies suspicious patterns and potential fraud, safeguarding financial integrity.
Workflow automation, routing, and triage
Efficiently manages claim assignments, escalations, and communications, ensuring smooth operations.
Analytics, audit trails, and reporting
Provides dashboards and reports for operational oversight, regulatory compliance, and performance tracking.
What to Consider When Purchasing AI Insurance Claims Processing Software
When evaluating AI claims processing software, insurers should consider factors that impact adoption, ROI, and operational efficiency.
-
Data privacy, security, and regulatory compliance: Ensure platforms comply with Health Insurance Portability and Accountability Act (HIPAA) and other regulations, with robust encryption and access controls.
-
Integration with existing systems and workflows: The software should connect seamlessly with EHRs, billing systems, and other operational tools.
-
Accuracy and error handling: Complex claims require hybrid workflows to maintain decision quality and transparency.
-
Vendor reputation, support, and scalability: Select vendors with proven track records, responsive support, and the ability to scale as claim volumes grow.
-
Cost vs. ROI and business case validation: Consider implementation and ongoing costs versus anticipated savings in efficiency, error reduction, and faster reimbursements.
Optimizing Health Insurance Claims with AI: The Path Forward
AI insurance claims processing is no longer optional. It is an essential component of modern health insurance operations. By leveraging automation, intelligent data extraction, and streamlined workflows, insurers can reduce costs, enhance accuracy, and improve satisfaction for both policyholders and providers.
For organizations seeking a robust and scalable solution, Aptarro’s RevCycle Engine offers a proven, end-to-end platform designed to optimize claims management. From hybrid workflows to actionable insights, it enables insurers to modernize operations while maintaining compliance and control.
Ready to transform your health insurance claims operations? Book a demo with Aptarro today and see how the RevCycle Engine can streamline your claims workflow, reduce errors, and accelerate reimbursements.
Author
